In vitro shear bond strength of 2 resin cements to zirconia and lithium disilicate: An in vitro study
Zirconia (ZrO2) ceramic resto- rations have become popular because of their metal-free structure, biocompatibility,1,2 and high fracture strength and fracture toughness.2,3 ZrO2 occurs as different for- mulations depending on the chemical composition and amount of the stabilizer, yttrium cation-doped tetra- gonal zirconia polycrystal (3Y-TZP), magnesium cation- doped partially stabilized zir- conia, and zirconia-toughened alumina.1,4 The disadvantages of ZrO2 ceramic restorations include an opaque appearance, the potential for fracture of the layered porcelain, inadequate marginal fit,5 and poor adhe- sion of resin cement.6-8
The surface properties of ZrO2 have been modified to improve its shortcomings. Yttria (Y2O3) was added to ZrO2 during firing to stabilize the crystal transformation and to improve its physical properties.1,2 The refractive index of ZrO2 is influenced by the orientation of the tetragonal crystals of the ZrO2. The high number of small crystalline grain in 3Y-TZP produces a high number of interfaces,
ABSTRACT
Statement of problem. There is little evidence on how the multiple layers of zirconia (ZrO2) or glazed material will affect the shear bond strength (SBS) of different resin cements.
Purpose. The purpose of this in vitro study was to compare the SBS of 2 resin cements with the different layers of a monolithic polychromatic ZrO2 ceramic, both glazed and nonglazed, and a lithium disilicate (LDS) ceramic.
Material and methods. One hundred and sixty-eight composite resin cylinders and 48 monolithic polychromic ZrO2 plates were prepared. Twenty-four were milled and sintered, and 24 were milled and sintered and had a glaze cycle applied with no liquid glaze. These plates and 12 LDS plates were mounted in autopolymerized acrylic resin. Bonding surfaces were polished, airborne- particle abraded, and cleaned ultrasonically. The different layers (cubic, hybrid, and tetragonal) of the ZrO2 plates were identified and marked. The plates were assigned to 2 cement groups: a self-adhesive, autopolymerized resin cement, and a dual-polymerizing, adhesive resin cement (DPRC). Bonding surfaces were cleaned and treated according to the cement manufacturer’s instructions. Three composite resin cylinders were luted to the ZrO2 plates at the appropriate layer, and 2 cylinders were luted to each LDS plate. The specimens were stored in a moist environment for 24 hours at 37 ◦C. The SBS test was performed with a universal testing machine. Visual inspections of the debonded surfaces were compared under magnification. The data were analyzed with a 2-way ANOVA and a subsequent Student t test (a=.05).
Results. The 2-way ANOVA found no difference among luting agent and LDS and ZrO2. The SBSs of the nonglazed tetragonal and cubic layer to the ZrO2 were higher than to the surface exposed to a glazing cycle (P=.001). The bonded surfaces were examined tactilely and under ×3.5 magnification, followed by light and scanning electron microscopy and recorded as either adhesive, cohesive, or mixed. Almost all failures in the glazed ZrO2 were mixed and cohesive. However, more adhesive failures were observed in the DPRC group of nonglazed ZrO2.
Conclusions. No differences were found between the 2 luting agents for the LDS. For the ZrO2 cubic and tetragonal layers, the DPRC had higher bond strengths to the nonglazed surfaces. (J Prosthet Dent 2021;125:529-34)
Supported by a grant from Mr and Mrs Norman Pessin.
a Adjunct Clinical Assistant Professor, Department of Prosthodontics, New York University College of Dentistry, New York, N.Y.
Professor Emeritus, New York University, New York, N.Y.
Clinical Associate Professor, Director Advanced Education Program in Prosthodontics, Department of Prosthodontics, New York University College of Dentistry, New York, N.Y.
Professor, Department of Biomaterials and Department of Basic Science and Craniofacial Biology, New York University College of Dentistry, New York, N.Y.
Clinical Implications
Resin cements are suitable luting agents for ZrO 2 restorations.
which scatter passing light and result in an opaque appearance.9 To address this optical disadvantage, 4Y- TZP and 5Y-TZP were developed by increasing the content of Y2O3. 4Y-TZP has 6.5 to 8 wt% Y2O3 (4 mol
%), whereas 5Y-TZP has 9 to 10 wt% Y2O3 (5 mol%). The quantity of the cubic phase is increased about 25% in 4Y-TZP to up to 50% in 5Y-TZP. Increasing the cubic phase with its larger grain size results in fewer grain boundaries, less birefringence, and a reduction in scat- tered light, increasing translucency.1,4 The high tetrag- onal phase content affords good mechanical properties yet yields optical disadvantages, which Zhang9 reported could be overcome by reducing its grain size.
New ZrO2 products have gradient layers starting from 4Y-TZP to 5Y-TZP with a hybrid layer in between. The 4Y-TZP layer contains 25% cubic phase and 75% tetragonal phase. The 5Y-TZP layer consists of 50% cubic phase and 50% tetragonal phase to impart more translucency.1,4
In spite of the research on ZrO2, the best method to promote a durable bond to ZrO2 is still controversial.2,8,10 In silica-based ceramics, such as feldspathic and lithium disilicate (LDS), microretention is primarily attained by chemical etching with hydrofluoric acid and applying a silane coupling agent.10 However, the composition and physical properties of ZrO2
silica-based ce- ramics so that hydrofluoric acid etching has no effect on the ZrO2 surface, and airborne-particle abrasion is the preferred surface treatment.10-13 Keshvad and Hakima- neh14 tested the microtensile bond strength of a resin cement to LDS and ZrO2 ceramic blocks and reported that the groups treated with laser irradiation had signif- icantly lower bond strengths.
Studies have reported that resin cements are the preferred method for luting ZrO2.10-13 A meta-analysis of
161 in vitro studies15 categorized into 3 groups of nonage, intermediate aged, and aged concluded that the diversity of methodology made comparisons difficult.
Newly developed self-adhesive resin cements have eliminated the need for etching, priming, and bonding as separate steps. Self-adhesive resin cements combine the high strength and low solubility advantages of resin ce- ments with the characteristic ease of use of self-adhesive systems, making them attractive to the clinician.16 A systematic review by Maroulakos et al17 found com- parable survival rates and complication patterns with ZrO2 and LDS tooth-supported complete-coverage res- torations after adhesive or conventional cementation,

Figure 1. Zirconia showing 3 layers. ZC, 50% cubic zirconia, 50% tetragonal zirconia; ZH, Hybrid zirconia, ZT, 25% cubic zirconia, 75% tetragonal zirconia.
which seems to indicate that loss of retention in ZrO2 restorations is not commonly encountered.
ZrO2 restorations are typically milled with computer- aided design and computer-aided manufacturing tech- nology; however, when a dentist receives a milled restoration from multilayered ZrO2 disks, it is difficult to tell which layer, or layers, make up the intaglio surface of the restoration and whether these different compositions influence the shear bond strength (SBS). In addition, many clinicians prefer to insert a glazed restoration. The problem is that there is little evidence on how the mul- tiple layers of the ZrO2 or the glazed material will affect the SBS of different resin cements.
The purpose of this in vitro study was to compare the SBS of 2 resin cements to each layer of a glazed and nonglazed polychromatic monolithic ZrO2 ceramic and an LDS ceramic. The research hypothesis was that the SBS of the tested luting agents (LAs) would be similar when bonded to the different layers of ZrO2 and to LDS.
MATERIAL AND METHODS
Composite resin (Tetric EvoCeram, Lot# W32425; Ivoclar Vivadent AG) cylinders (N=168) with a diameter of 2.38 mm and a height of 3mm height were prepared by packing the composite resin into Teflon molds (Ultradent Products, Inc) with hand pressure. They were light polymerized for 20 seconds by using a broad-spectrum polymerizing light (Bluephase Style 20i; Ivoclar Viva- dent AG).
Forty-eight (15×18×1.5 mm) polychromatic mono- lithic ZrO2 plates (IPS e.max ZirCAD MT Multi, Lot# W08468 Ref# 686887; Ivoclar Vivadent AG) were pre- pared (Fig. 1). Twenty-four were milled and sintered, and 24 were milled, sintered, and put through a glazing cycle with no liquid glaze applied. In addition, 12 (15×15×1.5 mm) LDS plates (IPS e.max CAD, Lot# V29465 Ref # 605330; Ivoclar Vivadent AG) were milled and sintered.
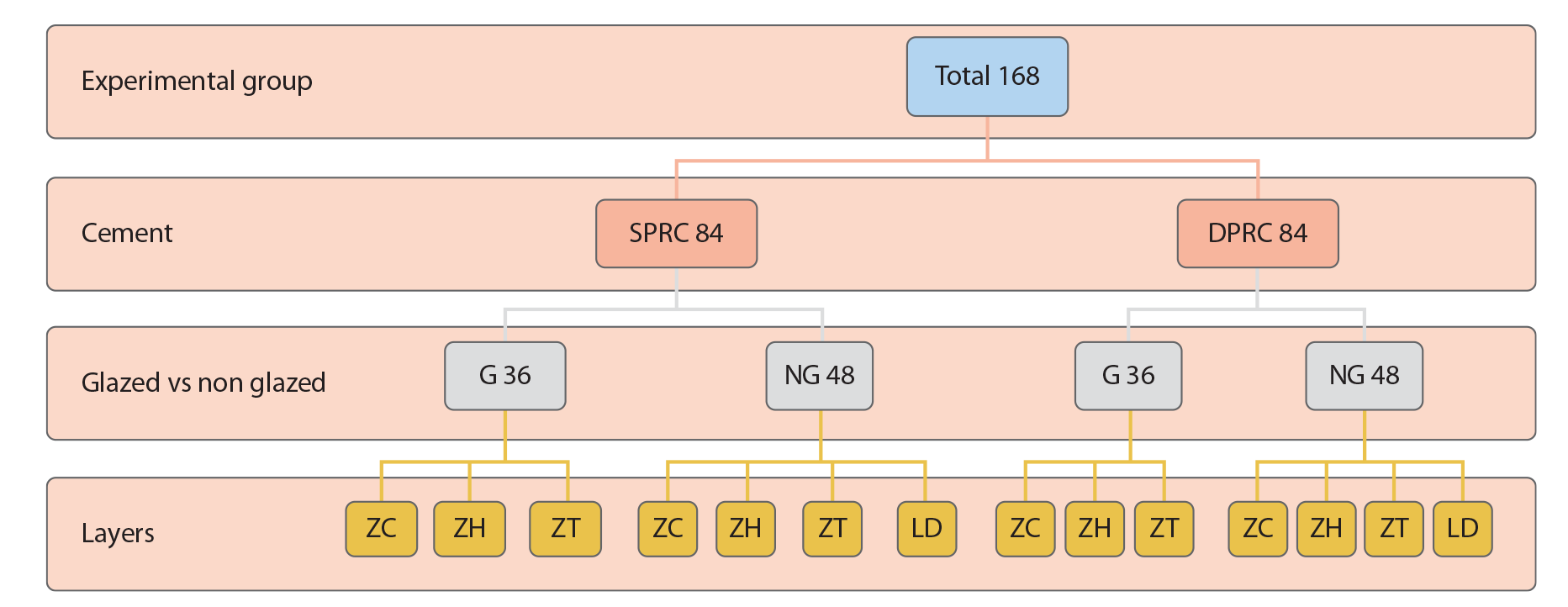
Figure 2. Schematic representation of testing groups. DPRC, dual-polymerizing, adhesive resin cement; SPRC, self-adhesive, autopolymerized resin cement; ZC, 50% cubic zirconia, 50% tetragonal zirconia; ZH, Hybrid zirconia, ZT, 25% cubic zirconia, 75% tetragonal zirconia
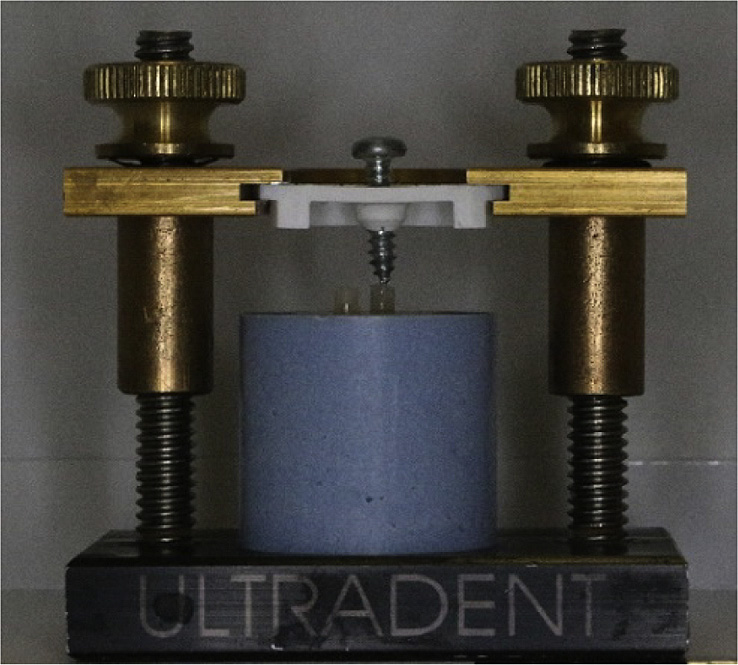
Figure 3. Bonding resin cylinder to test plates with modified device.
All plates were embedded in a 26-mm-diameter × 24-mm-high autopolymerizing acrylic resin (Bosworth Fastray, Lot# GG4558 DEN-001560; Keystone In-dustries). The bonding surfaces were then polished with 400-grit silicon carbide paper (EcoMet 250 grinder-polisher system; Buehler) with water, airborne-particle abraded with 50-mm aluminum oxide at 0.1 MPa pressure, and then cleaned ultrasonically for 10 minutes (Cristófoli Equipamentos de Biossegurança). Layers on the ZrO2 plates were identified with a hand-light and marked on the side of the mounting block. The plates were divided into 2 groups. A self-adhesive, autopolymerizing composite resin cement (Speedcem Plus, Lot # W38875; Ivoclar Vivadent AG) was used on 84 specimens, and a dual-polymerizing, adhesive composite resin cement (G-Cem LinkForce, Lot #1611181; GC America) was used on 84 specimens (Fig. 2). The bonding surface of the LDS was etched with 4.5% hydrofluoric acid (Lot# U19310; Ivoclar Vivadent AG) for 20 seconds, washed thoroughly with water, air dried, and a universal cleaning paste
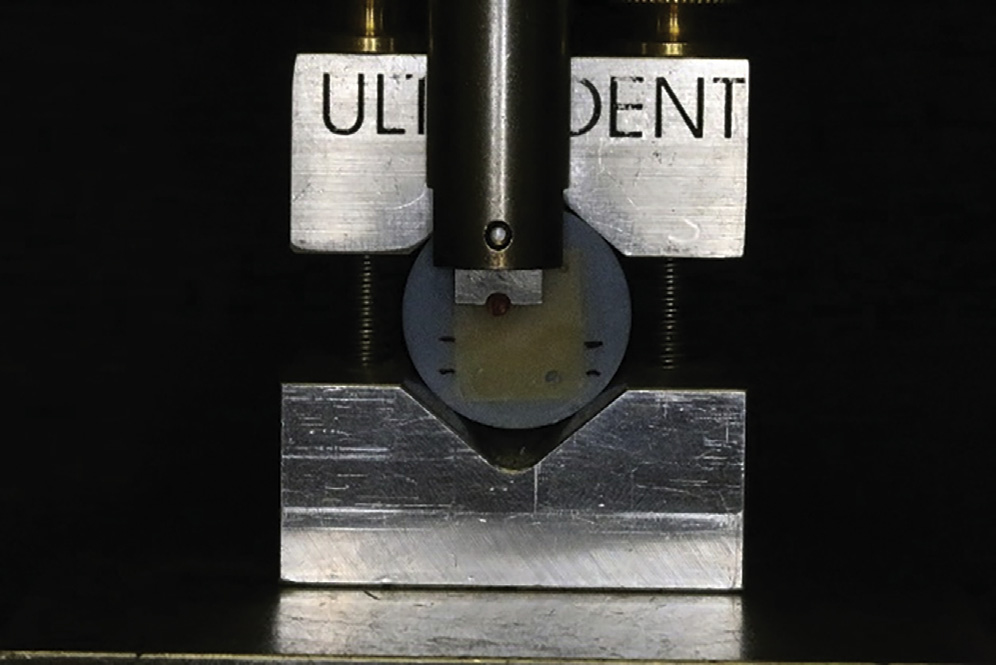
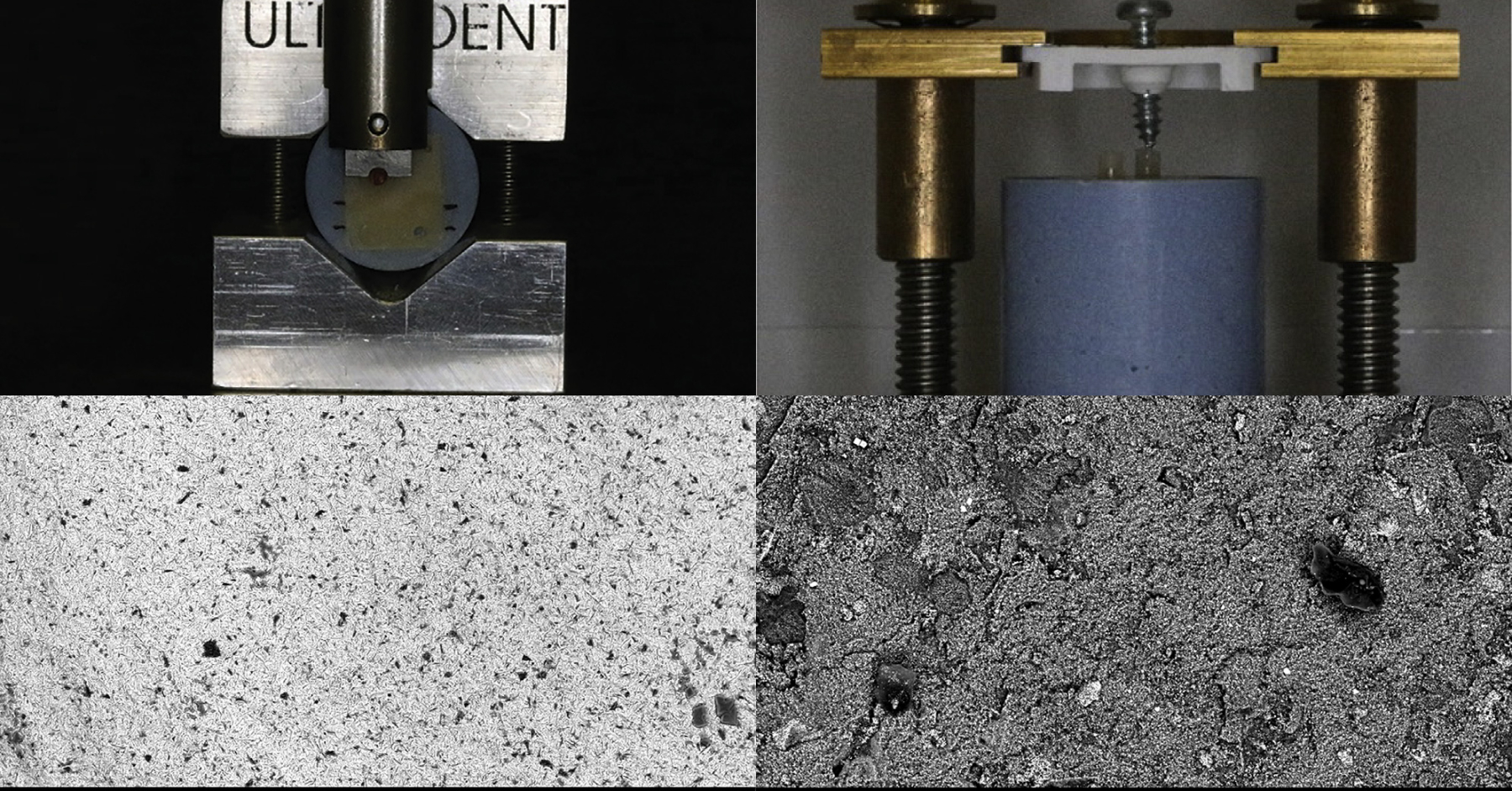
Figure 4. Shear bond strength testing.
(Ivoclean, Lot# W14374; Ivoclar Vivadent AG) was applied to the bonding surface of the ZrO2 and LDS plates for 20 seconds then washed with water and air dried. A primer (G-Multi primer, Lot #1611181; GC America) was applied on the ZrO2 plates tested for dual-polymerizing, adhesive resin cement (DPRC) and then air dried. For the LDS in the self-adhesive, auto-polymerized resin cement (SPRC) group, a primer (Monobond Plus, Lot# V33449; Ivoclar Vivadent AG) was applied to the bonding surface and then air dried.
Three composite resin cylinders were attached to each ZrO2 plate (1 on each layer) and 2 cylinders to the LDS plates. A small amount of LA was freshly dispensed each time, and the tip of the resin cylinder was dipped into the LA and then gently placed on the plates. A constant force was applied to the cylinder by means of the modified bond device (Ultradent Products, Inc) (Fig. 3); excess cement was removed with a microbrush (GC Corp), and the LA light polymerized for 20 seconds. The specimens were stored in a 37 C moist environment for 24 hours but were not allowed to contact the water. The SBS was
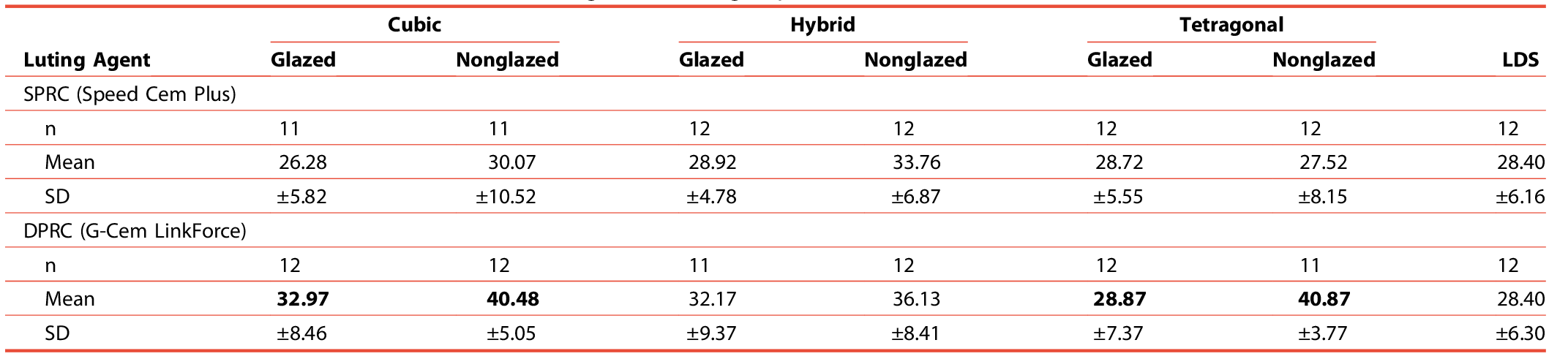
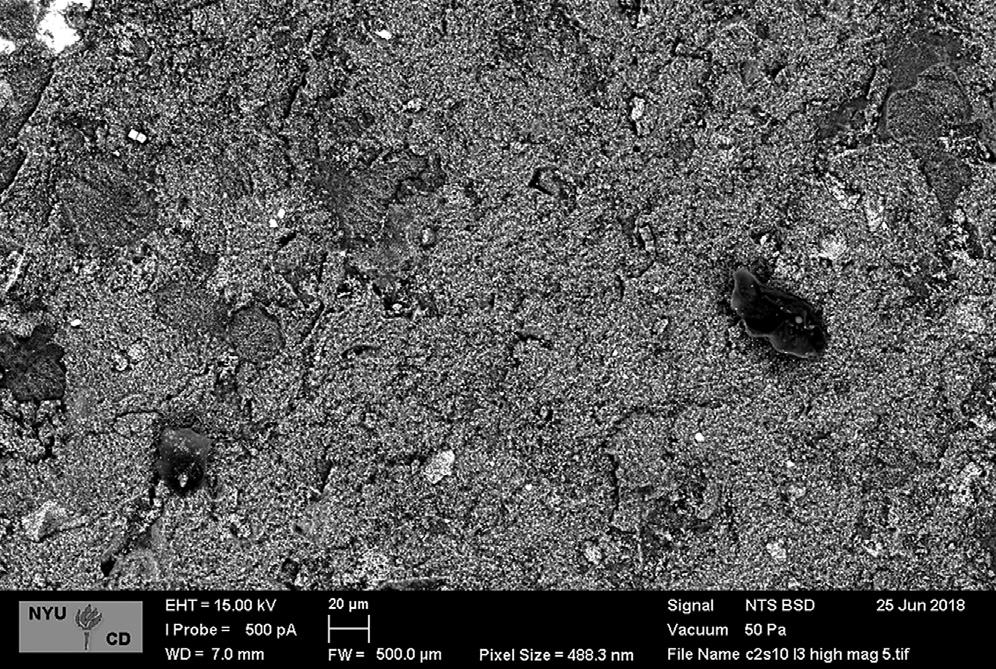
Figure 5. Cohesive failure showing luting agent on surface of ZrO2. See data zone for experimental details.
tested in a universal testing machine (3300; Instron Corp) (Fig. 4) at a crosshead speed of 1 mm/min.
Failure mode (adhesive, cohesive, or mixed) was iden-tified by examining the LA, ZrO2, and LDS surfaces with ×3.5 magnification loupes along with tactile analysis, an MZ APO (Leica) stereo light microscope, and, at variable pressure, in a scanning electron microscope (SEM) (EVO VP; Zeiss). Specimens with less than 10% residual LA were deemed an adhesive failure.18 The bond strength data were statistically analyzed by a 2-way ANOVA test (a=.05) and Student t tests (a=.01) by using a statistical software pro-gram (IBM SPSS Statistics, v24; IBM Corp).
RESULTS
Four specimens from the different test groups were excluded from analysis because of mechanical flaws: 1 from the SPRC cubic layer and 1 from the DPRC tetragonal layer in the nonglazed ZrO2 group and 1 from the SPRC cubic layer and 1 from the DPRC hybrid layer in the glazed ZrO2 group. The 2-way ANOVA found no significant difference between the LAs or the substrates tested (Table 1). The SBSs to the nonglazed tetragonal and cubic layer of the ZrO2 were higher than to the surface exposed to a glazing cycle (P=.001).
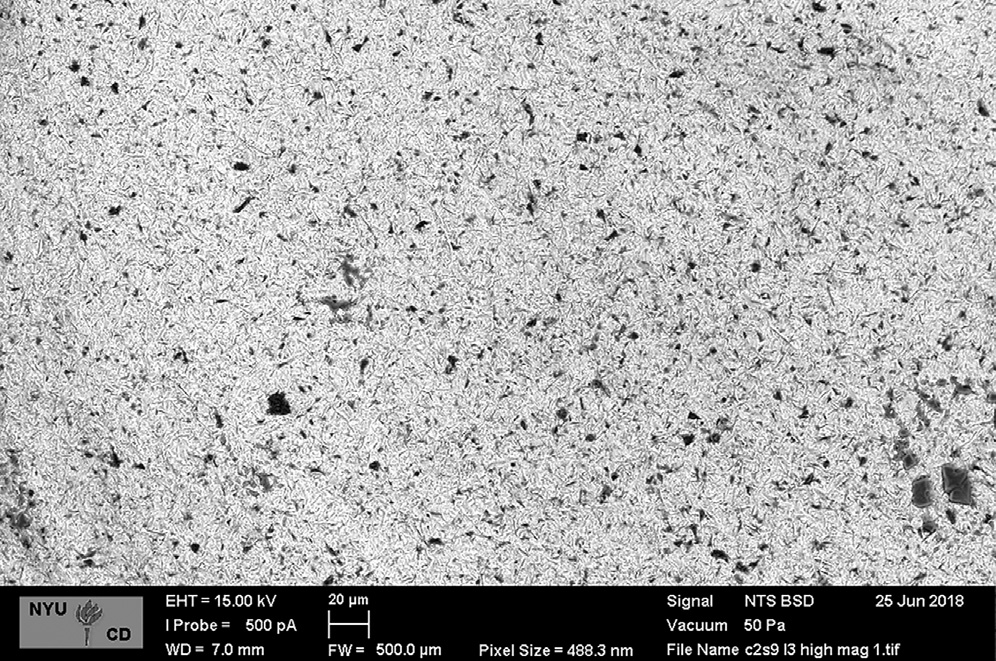
Figure 6. Adhesive failure showing residual primer on surface of ZrO2.
See data zone for experimental details.
Figure 5 shows a cohesive failure with LA present, and Figure 6 shows an adhesive failure with residual primer on the surface. When using SEM at higher magnification, no ZrO2 surfaces were totally free of LA. Figure 7 shows the mode of failure results for the ZrO2, and Figure 8 shows the LDS under ×3.5 magnification and with tactile eval-uation; almost all failures in the glazed ZrO2 were either mixed or cohesive. However, more adhesive failures were observed in the DPRC group of nonglazed ZrO2.
DISCUSSION
This study found clinically acceptable SBSs for the 2 LAs and the 2 substrates tested, confirming the research hy-pothesis. This finding was consistent with that of Maroulakos et al17 and anecdotal evidence from clini-cians reporting that retention of ZrO2 restorations is not a prevalent problem. The higher SBS of the DPRC to the nonglazed ZrO2 surfaces was unexpected and difficult to explain.
The methodology useddnot immersing the LA in water and not thermal cyclingdmay be the reason for the results. An LA should not be wet. Clinicians go to great lengths to ensure that the abutment tooth is dried and isolated. Once the LA polymerizes, the margins are sealed,
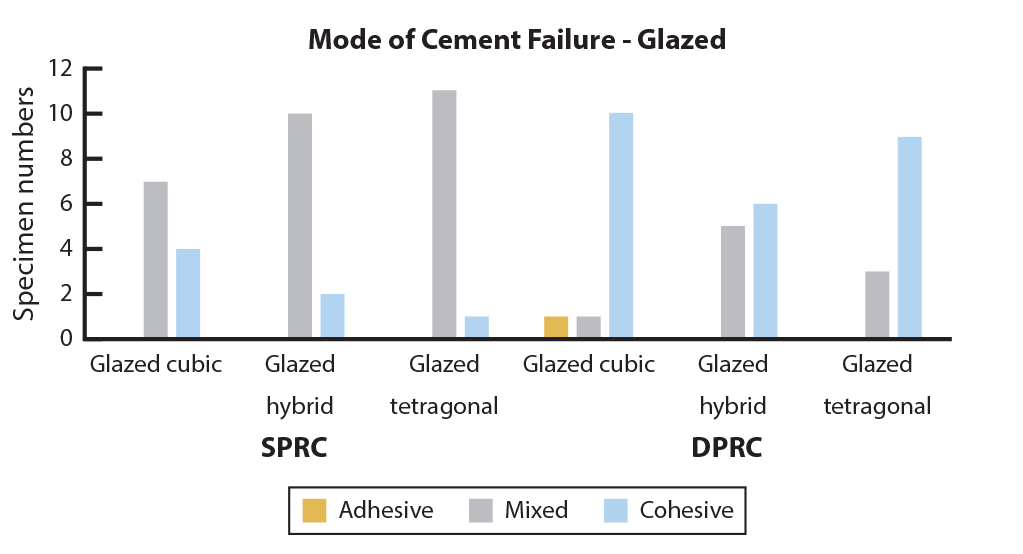
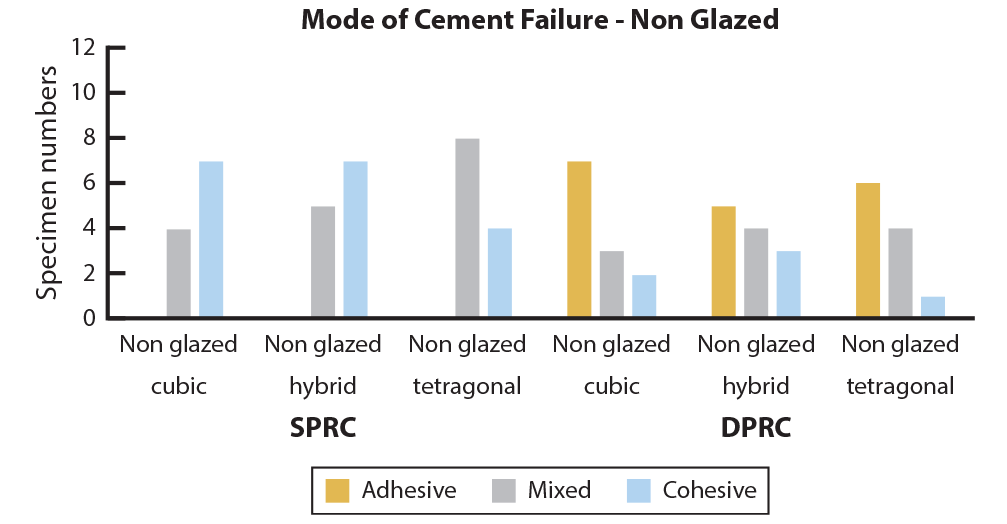
Figure 7. Mode of cement failure for zirconia by specimen numbers. DPRC, dual-polymerizing, adhesive resin cement; SPRC, self-adhesive, autopolymerized resin cement.
and moisture should not compromise the LA-to-tooth interface. A properly fabricated restoration with good marginal adaptation will not allow the LA to be exposed to saliva. It creates a seal that ensures the intaglio surface of the restoration is dry. The 25-mm to 100-mm pre-cementation space is exposed to oral liquids, but a major property of a reliable LA is low solubility,16 which would prevent that from happening in a properly fabricated and luted restoration. Patients function soon after receiving a restoration, so the ability of an LA to function immediately is essential. In this study, the specimens were exposed to a short-term storage regime of 37 C humidity for 24 hours to simulate the oral environment.
Thermal cycling is a time tested and universally accepted method of inducing thermal stress to simulate aging in in vitro dental studies. While thermal cycling has been reported to be valid for numerous studies, testing an LA in an open, wet environment, something that does not happen in vivo, is questionable. In addition, ZrO2 has low thermal conductivity and, unlike metals, would protect the LA from thermal changes; hence, the decision not to use thermal cycling in the present study.
Dérand and Dérand6 reported lower SBS values by using a similar methodology but with different LAs and a different substrate. The SBSs reported were higher for specimens stored for 1 week, whereas those stored for 2 months had varied results with 1 LA increasing while another decreased. Stefani et al7 reported similar re-sults and also did not thermal cycle, but they did use a
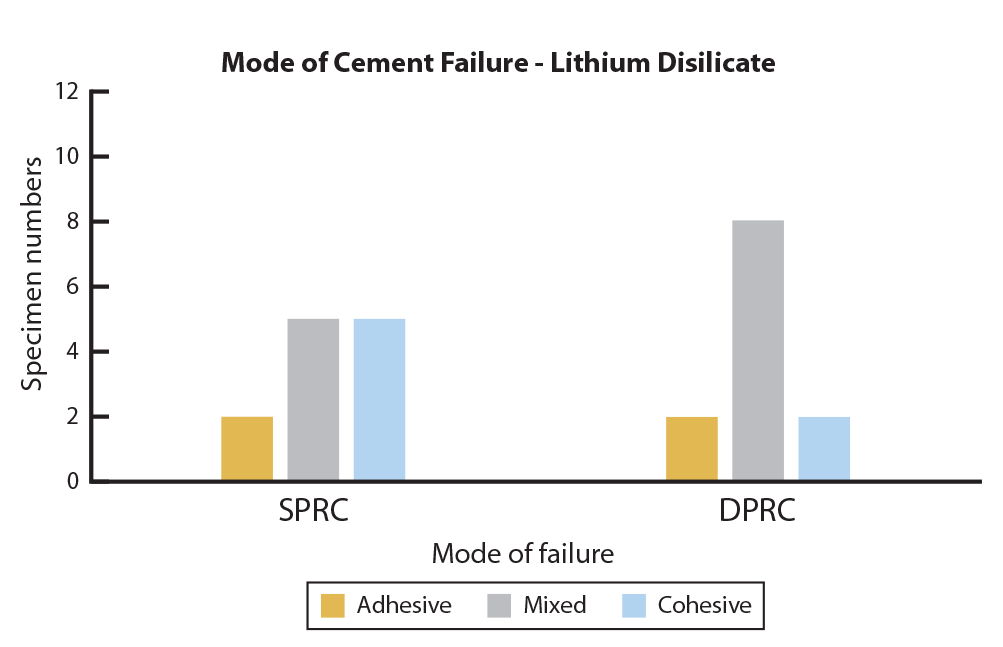
Figure 8. Mode of cement failure for lithium disilicate by specimen numbers. DPRC, dual-polymerizing, adhesive resin cement; SPRC, self-adhesive, autopolymerized resin cement.
24-hour immersion in 37 C water. Ebeid et al13 re-ported a decrease in tensile bond strength with aging in 37 C water and thermal cycling. A consensus on which test is most appropriate for this type of study is lacking, with some authors using SBS and others using tensile, micro shear, microtensile, and flexural strength testing.2
While it is possible to lute a nonglazed polished, ZrO2 restoration, clinicians also lute glazed ZrO2 restorations. In practice, the intaglio surface is not coated with a glazing liquid, but the restoration is still subjected to the heat of that procedure. The present study found that whether a ZrO2 surface went through a glazing cycle had an effect on the SBS with one of the tested LAs.
Whether a failure is adhesive or cohesive is important in planning improvements needed in future generations of the LA, the substrate, and/or the surface treatment to increase the bond strength. In the present study, an ad-hesive mode of failure was observed only in the DPRC group, in which an additional primer was used, with a dramatic increase in the nonglazed specimens, which also had higher SBSs. There are ranges of mixed failure and disagreement on how to distinguish between a mixed and adhesive failure.18 Some particles of LA are always present when the magnification of SEM images is increased. The present study reports the results under ×3.5 and tactile examination for adhesion and cohesion. The introduction of multilayered ZrO2 to achieve better esthetics creates 3 distinct layers, and because the clinician can never be certain of exactly how much of which layer is on the in-taglio surface after milling, this study evaluated the 3 layers separately and found no difference. Future clinical studies of luted ZrO2 restorations focusing on the LA and surface treatment are warranted.
CONCLUSIONS
Based on the findings of this in vitro study, the following conclusions were drawn:
- No differences were found between the 2 LAs for the LDS.
- For the ZrO2 cubic and tetragonal layers, the dual-polymerizing, adhesive composite resin cement had higher bond strengths to the nonglazed surfaces.
REFERENCES
- Kelly JR, Denry I. Stabilized zirconia as a structural ceramic: an overview. Dent Mater 2008;24:289-98.
- Bona AD, Pecho OE, Alessandretti R. Zirconia as a dental biomaterial. Ma-terials 2015;8:4978-91.
- Yilmaz H, Aydin C, Gul BE. Flexural strength and fracture toughness of dental core ceramics. J Prosthet Dent 2007;98:120-8.
- Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater 2008;24:299-307.
- Encke BS, Heydecke G, Wolkewitz M, Strub JR. Results of a prospective randomized controlled trial of posterior ZrSiO(4)-ceramic crowns. J Oral Rehabil 2009;36:226-35.
- Dérand P, Dérand T. Bond strength of luting cements to zirconium oxide ceramics. Int J Prosthodont 2000;13:131-5.
- Stefani A, Brito RB, Kina S, Andrade OS, Ambrosano GMB, Carvalho AA, et al. Bond strength of resin cements to zirconia ceramic using adhesive primers. J Prosthodont 2016;25:380-5.
- Chai H, Kaizer M, Chughtai A, Tong H, Tanaka C, Zhang Y. On the inter-facial fracture resistance of resin-bonded zirconia and glass-infiltrated graded zirconia. Dent Mater 2015;31:1304-11.
- Zhang Y. Making yttria-stabilized tetragonal zirconia translucent. Dent Mater 2014;30:1195-203.
- Kern M, Wegner SM. Bonding to zirconia ceramic: Adhesion methods and their durability. Dent Mater 1998;14:64-71.
- Shahin R, Kern M. Effect of air-abrasion on the retention of zirconia ceramic crowns luted with different cements before and after artificial aging. Dent Mater 2010;26:922-8.
- Gargari M, Gloria F, Napoli E, Pujia AM. Zirconia: cementation of prosthetic restorations. Literature review. Oral Implantol (Rome) 2010;3: 25-9.
- Ebeid K, Wille S, Salah T, Wahsh M, Zohdy M, Kern M. Bond strength of resin cement to zirconia treated in pre-sintered stage. J Mech Behav Biomed Mater 2018;86:84-8.
- Keshvad A, Hakimaneh SMR. Microtensile bond strength of a resin cement to silica-based and Y-TZP ceramics using different surface treatments. J Prosthodont 2018;27:67-74.
- Thammajaruk P, Inokoshi M, Chong S, Guazzato M. Bonding of composite cements to zirconia: A systemic review and meta-analysis of in vitro studies. J Mech Behav Biomed Mater 2018;80:258-68.
- Manso AP, Carvalho RM. Dental cements for luting and bonding restorations self-adhesive resin cements. Dent Clin N Am 2017;61:
- Maroulakos M, Thompson GA, Kontogiorgos ED. Effect of cement type on the clinical performance and complications of zirconia and lithium disilicate tooth-supported crowns: A systematic review. Report of the Committee on Research in Fixed Prosthodontics of the American Academy of Fixed Prosthodontics. J Prosthet Dent 2019;121: 754-65.
- Scherrer SS, Cesar PF, Swain MV. Direct comparison of the bond strength results of the different test methods: A critical literature review. Dent Mater 2010;26:e78-93.
Corresponding author:
Dr Gary Goldstein
One UN House SIDS St, Tuana’imato
SAMOA
Email: [email protected]
Acknowledgments
The authors thank Ivoclar Vivadent AG for their technical expertise and material assistance as well as GC America Inc for material assistance.
Copyright © 2020 by the Editorial Council for The Journal of Prosthetic Dentistry. https://doi.org/10.1016/j.prosdent.2020.02.020